Virus-free CRISPR could mean faster, more precise gene editing for T-cell therapies
A team from the University of California, San Francisco, devised a new electroporation-based CRISPR-Cas9 method, eliminating viruses from the gene editing process and laying the groundwork for safer, more precise and more efficient editing for CAR-T cancer treatments and other cell therapies.
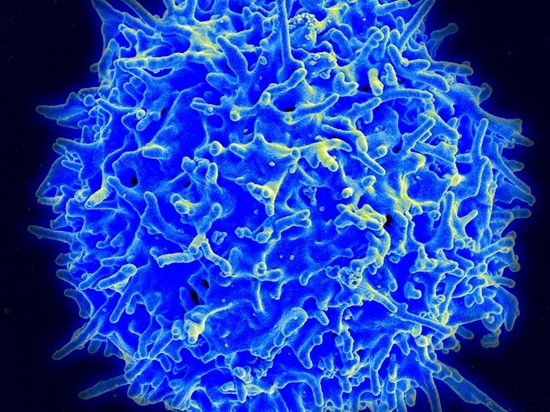
A team from the University of California, San Francisco, devised a new electroporation-based CRISPR-Cas9 method, eliminating viruses from the gene editing process and laying the groundwork for safer, more precise and more efficient editing for CAR-T cancer treatments and other cell therapies.
The researchers believe the approach could address the shortcomings of virus-based editing, a time-consuming process that inserts genes into the T-cell genome with limited predictability. Producing viruses for cell therapies—such as lentiviruses for CAR-Ts—can take as long as a year, which slows down research and increases the time a patient must wait before receiving treatment, they said in a statement.
But a major barrier to the nonviral editing of T cells has been the toxicity of the DNA sequences to be inserted into the target genome. The researchers found that using electroporation—a process that makes cell membranes temporarily more permeable—reduced toxicity, allowing them to cut and paste specific sequences precisely at the site of a CRISPR-programmed cut in the genome.
Along with colleagues from UCLA's Parker Institute for Cancer Immunotherapy, the team used the method to replace a native receptor in human T cells with a new receptor engineered to hunt down a specific subtype of melanoma cells. The modified T cells targeted and attacked melanoma cells in a lab dish while leaving other types of cells unharmed.
The researchers were also able to insert much longer pieces of DNA into T cells than previously possible, opening up more opportunities for engineered cell therapies. “With the ability to rewrite long stretches of DNA—over 1,000 nucleotides at a time—we can start making more significant genetic changes to T-cells and make them more efficient at recognizing cancer and killing cancer,” said senior author Alexander Marson, M.D., Ph.D., an associate professor of microbiology and immunology at UCSF, in a UCLA release. The findings appear in Nature.
Much work is under way to make CAR-Ts safer, including the development of built-in safety switches to control CAR-T activity and the use of multiple target antigens to make CAR-Ts more effective in solid tumors.
The electroporation method could be broadly applicable, not just in CAR-T and cell therapy, but also in gene-editing research targeted at inherited diseases. Adeno-associated viruses are the most common CRISPR vector, but they allow CRISPR components to persist in cells after editing is complete, leaving them vulnerable to off-target mutations. And because they are too small to encapsulate all three CRISPR components—a guide RNA, enzyme and donor DNA—a large dose of viruses is required to deliver the therapy.
The UCSF researchers tested their approach in T cells taken from three siblings with a rare autoimmune disease. They repaired a defect in the cells' IL2RA gene, restoring cellular signals involved in the development of regulatory T cells (Tregs), which control other immune cells and prevent autoimmunity. The researchers hope this approach could extend to other autoimmune diseases in which Tregs malfunction.
Link: Fierce Biotech


ارسال به دوستان