Second patient free of HIV after stem-cell therapy
The breakthrough suggests first case was not a one-off and could pave way for future treatments.
A person with HIV appears to be free of the virus after receiving a stem-cell transplant that replaced their white blood cells with HIV-resistant versions. The patient is only the second person ever reported to have been cleared of the virus using this method. But researchers warn that it is too early to say that they have been cured.
The patient — whose identity hasn’t been disclosed — was able to stop taking antiretroviral drugs, with no sign of the virus returning 18 months later. The stem-cell technique was first used a decade ago for Timothy Ray Brown, known as the ‘Berlin patient’, who is still free of the virus.
So far, the latest patient to receive the treatment is showing a response similar to Brown, says Andrew Freedman, a clinical infectious diseases physician at Cardiff University who was not involved in the study. “There’s good reason to hope that it will have the same result,” he says.
Like Brown, the latest patient also had a form of blood cancer that wasn’t responding to chemotherapy. They required a bone-marrow transplant, in which their blood cells would be destroyed and replenished with stem cells transplanted from a healthy donor.
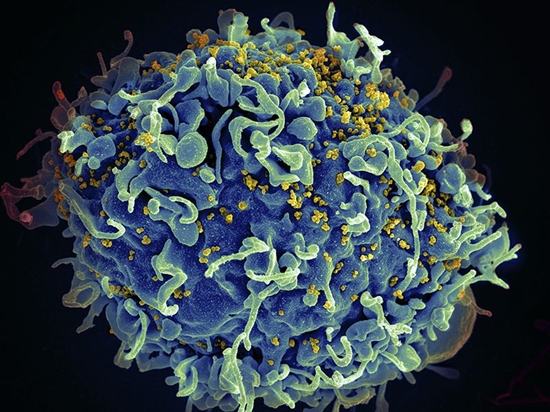
But rather than choosing just any suitable donor, the team, led by Ravindra Gupta, an infectious diseases physician at the University of Cambridge, UK, picked a donor who had two copies of a mutation in the CCR5 gene, which gives people resistance to HIV infection. This gene codes for a receptor which sits on the surface of white blood cells involved in the body’s immune response. Normally, the HIV binds to these receptors and attacks the cells, but a deletion in the CCR5 gene stops the receptors from functioning properly. About 1% of people of European descent have two copies of this mutation and are resistant to HIV infection.
Gupta’s team describes the results in a paper due to be published in Nature on 5 March. The researchers report that the transplant successfully replaced the patient’s white blood cells with the HIV-resistant variant. Cells circulating in the patient’s blood stopped expressing the CCR5 receptor, and in the lab, the researchers were unable to re-infect these cells with the patient’s version of HIV.
The team found that the virus completely disappeared from the patient’s blood after the transplant. After 16 months, the patient stopped taking antiretroviral drugs, the standard treatment for HIV. In the latest follow-up, 18 months after stopping medication, there is still no sign of the virus.
Aggressive treatment
Gupta says that it’s not yet possible to say whether the patient has been cured. This can only be demonstrated if the patient’s blood remains HIV-free for longer, he says.
But the study does suggest that Brown’s successful treatment 10 years ago wasn’t just a one-off. Gupta says that the latest patient received a less aggressive treatment than Brown to prepare for the transplant. The new patient was given a regimen consisting of chemotherapy alongside a drug that targets cancerous cells, while Brown received radiotherapy across his entire body in addition to a chemotherapy drug.
That suggests that, to be successful, stem-cell transplants in HIV patients would not necessarily need aggressive treatments that might have particularly severe side effects, says Gupta. “The radiation really does knock the bone marrow and make you very sick.”
Graham Cooke, a clinical researcher at Imperial College London, points out that this kind of treatment wouldn’t be suitable for most people with HIV — who don’t have cancer and so don’t need a bone-marrow transplant, which is a serious procedure that can sometimes have fatal complications. “If you’re well, the risk of having a bone-marrow transplant is far greater than the risk of staying on tablets every day,” he says. Most people with HIV respond well to daily antiretroviral treatment.
But Cooke adds that for those who need a transplant to treat leukaemia or other diseases, it seems reasonable to try and find a donor with the CCR5 mutation, which wouldn’t add any risk to the procedure.
Gero Hütter, who led Brown’s treatment and is now medical director of stem-cell company Cellex in Dresden, Germany, agrees that this kind of treatment could only ever be used for a small group of patients. But he hopes that the paper will stimulate a renewed interest in gene therapies that target CCR5, which could be applied to a much broader group. “The real breakthrough, we are still waiting for,” he says.
Link: doi: 10.1038/d41586-019-00798-3


ارسال به دوستان