Gene therapy for sickle cell disease steps closer
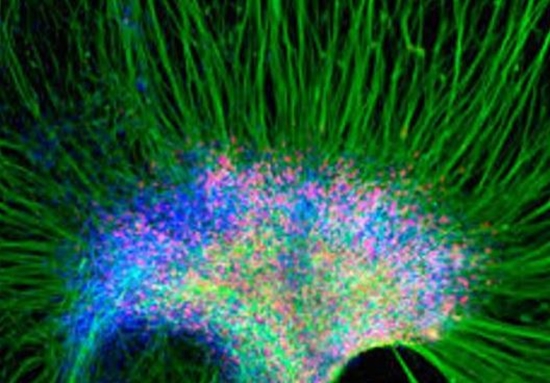
em cells can develop into many different types of cells, such as muscle cells, red blood cells, or neurons. Given their special regenerative ability, stem cells can be used to treat a wide range of diseases. A team of researchers uncovers new details involved in the process of turning stem cells into motor neurons.
In a study published in Nature, they report how - using the CRISPR gene-editing tool - they corrected the gene in stem cells from diseased patients and showed they could make red blood cells capable of making functioning hemoglobin. They also transplanted the stem cells into mice and found them thriving in their bone marrow months later.
Sickle cell disease is a group of inherited disorders where red blood cells form abnormal, hard and sticky, crescent, or sickle shapes instead of normal, flexible, disc-like shapes.
The sickle red blood cells stick to vessel walls and cause blockages, slowing the flow of blood and stopping oxygen reaching nearby tissues. This can cause pain and damage to tissue and organs. Also, sickle cells die faster than normal red blood cells, raising risk of anemia, which can also damage organs.
The disease is caused by a single mutation in a gene that codes for a protein chain in hemoglobin - the molecule in red blood cells that carries oxygen. The faulty hemoglobin forms stiff rods within the red cell, making it crescent-shaped.
Sickle cell disease affects millions of people around the world. The number of Americans living with it is not known, but estimates suggest it is around 100,000.
Children born with sickle cell disease in high-income countries typically survive and can go on to live full lives and enjoy most of the activities that other people do. However, in low-income countries, children born with the disease typically die before they reach their fifth birthday.
Gene therapy and the promise of CRISPR
Since its early beginnings in the 1980s, gene therapy has been a holy grail among researchers looking for ways to cure or treat genetic disorders.
CRISPR is a relatively new gene-editing tool that is said to have "triggered a revolution in genome engineering within living systems." Researchers prefer CRISPR to older methods because it is easier and faster.
The technique is a type of molecular scissors that snip out faulty strips of DNA so they can be replaced with corrected versions using other tools.
Matthew H. Porteus, associate professor of pediatrics at Stanford University, CA, and senior author of the new study, has been trying ways to target sickle cell genes with gene-editing technology for several years.
He says with the new CRISPR technology, they can work much faster and more effectively, significantly cutting the time of experiments.
"We spent half a dozen years trying to target the beta globin gene using the old technology," he remarks, adding that within a week of trying CRISPR, they had a gene-editing tool that was much better.
For their new study, Prof. Porteus and his team took hematopoietic stem cells from the blood of patients with sickle cell disease and corrected the faulty gene using CRISPR to remove a strip of DNA and a virus to insert the correct version. Hematopoietic stem cells are stem cells that make blood cells.
They concentrated the human hematopoietic stem cells so that 90 percent carried the corrected sickle cell gene and then injected them into young mice.
Proof of concept that gene-editing can repair sickle cell
Prof. Porteus says that the hematopoietic stem cells have the ability to travel from the bloodstream into the bone marrow, where they then "set up shop and start making other blood cells."
Sixteen weeks after the transplant, the researchers found the stem cells were thriving in the mice's bone marrow.
A gene therapy for sickle cell disease would not have to replace all of a patient's sickle cells Prof. Porteus explains. You just need a sufficient amount of normal cells. Patients whose sickle cells are below 30 percent show no symptoms of disease.
The researchers now need to take their discovery through a series of tests so they can investigate the safety aspects of the new gene editing tool.
This is going to be no mean feat - no CRISPR-edited genes have yet been tested for safety or efficacy in human clinical trials. A particular challenge is how to overcome potential so-called "off-target" effects, where the molecular scissors accidentally cut out the wrong piece of DNA.
Prof. Porteus says Stanford is building the infrastructure so they can start to take their findings out of the lab and scale them up into the types of systems that will be needed to create gene therapy for patients.
For now, he and his team can say that their gene-edited human hematopoietic stem cells appear to behave like normal, healthy human hematopoietic stem cells.
They suggest their findings are proof of concept that using gene-editing can repair sickle cell and other bloodborne genetic diseases, such as thalassemia.
"What we've finally shown is that we can do it. It's not just on the chalkboard. We can take stem cells from a patient and correct the mutation and show that those stem cells turn into red blood cells that no longer make sickled hemoglobin."
Prof. Matthew Porteus
http://www.medicalnewstoday.com/articles/313997.php


ارسال به دوستان